Current location: Home > NEWS > Corporate news
NEWS
PRODUCTS
Academic achievements - the application of molecular classification in guiding the care and fertility preservation treatment of patients with endometrial cancer or endometrial intraepithelial neoplasia Background of Fertility Preservation Treatment
News source: Release time:[2023-01-18]
Endometrial cancer (EC) is one of the most common malignant tumors of the female reproductive system. In 2016, there were 71,100 new cases of uterine cancer and 17,100 deaths in Chinese, most of which were EC. In recent years, the incidence of EC in China has increased, and the incidence of young women is on the rise, especially in developed cities. Up to 14% of patients are women who are at the reproductive age who are likely to have a favorable long-term prognosis and wish to preserve their fertility. With the changes in China's fertility policy and the increase in the number of young women delaying childbearing, the proportion of these patients is increasing. Conservative care is therefore an important requirement for these young women with EC [1].
According to the NCCN guidelines, the prerequisites for fertility preservation treatment are as follows: (1) well-differentiated (G1) endometrioid carcinoma (EEC) confirmed by a pathologist after diagnostic curettage; (2) magnetic resonance imaging (MRI) ) or transvaginal ultrasonography to confirm that the lesion is limited to the endometrium; (3) no other suspicious metastatic lesions in imaging examination; (4) no contraindications to drug treatment or pregnancy; (5) patients must be informed that fertility preservation treatment is not EC standard treatment [2]. Treatment is mainly with progestogen-based continuous therapy: oral megestrol acetate, medroxyprogesterone acetate, or the use of a levonorgestrel intrauterine device (LNG-IUS) [3].
Molecular Classification of Endometrial Cancer
The molecular classification of EC has been one of the hot topics in the field of gynecological tumors in the past two years. In 2013, The Cancer Genome Atlas (TCGA) included 373 EC patients with different tumor stages, histological types, tumor differentiation grades and adjuvant treatment methods. Using multi-omics detection methods, according to mutation types and copy number differences, EC can be Divided into 4 subtypes, namely POLE hypermutation type, microsatellite instability (MSI) hypermutation type, low copy number (CN-L) type and high copy number (CN-H) type. The study found that the progression-free survival (PFS) of the four subtypes was significantly different: the POLE mutant type had the best prognosis, the CN-H type had the worst prognosis, and the MSI type and CN-L type were in the middle (P=0.02)[4]. Subsequent studies such as ProMisE and TransPORTEC have obtained similar conclusions [5-6].
The TCGA study found that according to the results of mRNA sequencing, the expression of progesterone receptor (PGR) increased in CN-L tumors, suggesting that these patients may respond to hormone therapy. Further analysis found that, compared with the other three subtypes, the expression of PGR increased in the CN-L subtype, all with significant differences [4].
Research Progress in Foreign Countries
In a Korean study evaluating 57 patients receiving conservation therapy, mismatch repair deficient (MMRd) patients had a significantly lower complete response (CR) or partial response (PR) rate than p53 wild-type (p53wt) patients (44.4 % vs 82.2%, P=0.018), the CR rate at 6 months (11.1% vs 53.3%, P=0.01) and the cumulative CR rate (p=0.035) were also significantly different. Among patients with the MMRd type, 4 underwent immediate hysterectomy due to treatment failure, and 3 had diagnostic escalation after hysterectomy. The study concluded that molecular classification has prognostic significance in the fertility preservation management of EC and that MMR status can be used as a predictive biomarker for excluding patients who would benefit from hormone therapy [7].
Researchers in the United States found MMR protein loss in 6 patients (7%) aged ≤55 years with complex atypical hyperplasia of the endometrium or FIGO stage I EEC by immunohistochemistry (IHC). These patients had a higher incidence of invasive cancer and do not respond well to progestin therapy. The tumor regression rate of dMMR patients was 0, which was significantly different from that of patients with normal mismatch repair function (pMMR) (p=0.028). All 6 patients with dMMR eventually underwent surgery [8]. Another Italian study also found that dMMR patients were more commonly resistant to conservation therapy than pMMR patients (33.3% vs 15.9%), but this was not statistically significant (P=0.2508). The recurrence rate of dMMR patients was significantly more than that of pMMR patients (100% vs 26.4%, P<0.0001), and the specificity of dMMR in predicting recurrence reached 100%[9].
Allison M. Puechl et al. assessed whether molecular classification could predict response to LNG-IUS in patients with EC and endometrial intraepithelial neoplasia (EIN). According to the classification strategy of ProMisE, IHC was used to detect MMR and p53 proteins, and the sequencing method was used to detect the POLE exonuclease domain. Of the 58 patients enrolled in the study, 22 (37.9%) had EC and 36 (62.1%) had EIN; 44 (75.9%) were classified as p53wt type and 6 (10.3%) were classified as MMRd type, 4 cases (6.9%) were classified as p53 abnormal (p53abn) type, and 4 cases (6.9%) were classified as POLE mutant type. Eleven cases (19.0%) progressed (PD) or changed treatment methods, and the p53abn type progressed the fastest [10].
The Latest Domestic Research [1]
Recently, the Department of Pathology and Department of Obstetrics and Gynecology from Peking University Peoples Hospital have cooperated with XIAMEN SPACEGEN CO.,LTD. and used XIAMEN SPACEGEN CO.,LTD.’s endometrial cancer molecular classification test to evaluate the relationship between molecular classification and EEC or endometrial atypical hyperplasia/endometrial epithelium, the relationship between treatment response in women with internal neoplasia (EAH/EIN). Related research results were published in the journal PATHOL RES PRACT (IF=3.309).
The researchers performed a retrospective analysis of 39 EEC and 20 EAH/EIN patients who underwent fertility preservation treatment between 2013 and 2021. All patients received high-dose progesterone therapy (500 mg per day), monthly ultrasound monitoring, and quarterly hysteroscopy. The researchers performed IHC analysis on the biopsy samples, including p53 and MMR proteins (MSH2, MSH6, PSM2, MLH1), and used the endometrial cancer molecular classification kit independently developed by XIAMEN SPACEGEN CO.,LTD. for molecular detection.
The median age of the patients was 33.4 years. The median follow-up period of the study was 16.8 months, during which 4 patients gave up progesterone therapy due to PD. Among the 39 EEC patients, 23 achieved CR after fertility preservation treatment, which was significantly lower than that in the EAH/EIN group (58.97% vs. 80.0%, P<0.05). The samples of 59 patients were all molecularly classified, and the distribution of the 4 subtypes was as follows: 83.05% (49/59) were CN-L type, 6.78% (4/59) were MSI-H type, and each had 5.08% (3/59) of POLE hypermutated and CN-H types. The results of MSI and TP53 sequencing were consistent with the IHC analysis of MMR and p53 protein. The proportions of patients with each molecular subtype achieving CR were: 100% (3/3) for POLE hypermutation type, 71.43% (35/49) for CN-L type, and 25% (1/4) for MSI-H type , CN-H type is 33.3% (1/3). The prognosis of POLE hypermutation type and CN-L type is better than that of MSI-H type and CN-H type.
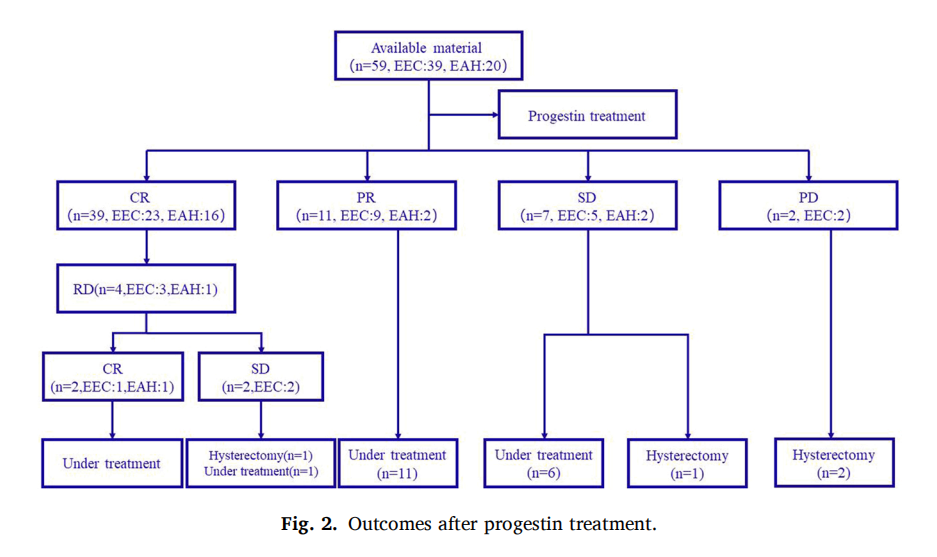
Results of Progestin Therapy
This study is one of the first studies to report the relationship between molecular subtypes and fertility preservation treatment results in women with EEC or EAH/EIN, and it is also the first similar study based on a Chinese population. The molecular classification of EAH/EIN has rarely been reported before. In this study, 20 cases of EAH/EIN were included, which met the requirements of quality control and obtained the classification results. More importantly, unlike previous researchers who focused on morphological changes, this study combined morphological and molecular assays to assess the relationship between molecular classification and prognosis during treatment and follow-up.

Result of patients with different histological types (A) and molecular subtypes (B)
Most of the samples in this study are CN-L type, which is related to the low-level EEC and EAH/EIN of the fertility preservation treatment patients. The prognosis of patients with MSI-H type is quite different, with CR, PR, recurrence (RD) and PD in 1 case each. This also confirmed that patients with MSI-H type were less sensitive to hormone therapy than patients with pMMR. CN-L and POLE mutations are more sensitive to the care and treatment, which may be related to higher levels of PGR expression. CN-H type is not sensitive to hormone therapy and has a poor prognosis. Although EAH/EIN and low-level EEC are relatively inert, the results of this study show that TP53 mutation and MSI-H status may predict poor treatment results.
Conclusion
Young patients with EAH/EIN or low-grade EEC who want to retain fertility can consider conservative treatment. Compared with EEC patients, EAH/EIN patients have better curative effect. Molecular classification of EAH/EIN is feasible. Molecular classification of EEC and EAH/EIN biopsy samples may predict patients at risk of progression before progesterone treatment [1].
The molecular classification of endometrial cancer of XIAMEN SPACEGEN CO.,LTD. adopts the high-throughput sequencing method to comprehensively detect the typing markers and auxiliary classification factors recommended by the guidelines, which can provide clues to the prognosis, adjuvant therapy, immunotherapy, hormone therapy and genetic risk of EC patients. XIAMEN SPACEGEN CO.,LTD. is committed to providing the most innovative products and services for personalized and accurate medical detection of tumors, and continuously updating existing products.
Reference
[1] Pathol Res Pract. 2022 Dec 19;241:154278.
[2] NCCN Guidelines for Clinical Diagnosis and Treatment of Uterine Tumors 2023 v1
[3] Guidelines for the Diagnosis and Treatment of Endometrial Cancer (2021 edition)
[4] Nature. 2013 May 2; 497(7447):67-73.
[5] Ann Oncol. 2018 May 1; 29(5): 1180-1188.
[6] J Clin Oncol. 2020 Oct 10; 38(29): 3388-3397.
[7] Am J Obstet Gynecol. 2021 Apr;224(4):370.e1-370.e13.
[8] BJOG. 2017 Sep;124(10):1576-1583.
[9] Gynecol Oncol. 2021 Jun;161(3):795-801.
[10] Cancers (Basel). 2021 Jun 7;13(11):2847.