Current location: Home > NEWS > Industry news
NEWS
PRODUCTS
Molecular Classification of G3 Endometrioid Carcinoma
News source: Release time:[2022-12-15]
Abstract
In the past two decades, the incidence of endometrial cancer (EC) has been increasing, which require molec
-ular markers to predict prognosis and guide treatment. TCGA studies have shown that the diagnosis, prognosis and treatment methods can be improved by EC molecular typing. Since then, more and more studies have confirmed this view, and molecular typing has also been included in various authoritative guidelines and consensuses.
Recently, the research result Molecular classification grade 3 endometrial endometrioid carcinoma using a next-generation sequencing-based gene panel was published online in the international journal "Frontiers in Oncology" by the Department of Gynecologic Oncology, Department of Molecular Pathology and Department of Pathology of Fujian Cancer Hospital. (Impact factor 5.738, 2022)) [1]. XIAMEN SPACEGEN CO.,LTD. participated in this research as a technical partner.
Background
Endometrial cancer (EC) is the sixth most common cancer among women worldwide. In recent years, the morbidity and mortality of EC have gradually increased. EC is the top 10 new cancers in women in China, ranking second among female reproductive system malignancies. In 2020, there will be 82,000 new cases of EC in China, accounting for 3.9% of female malignant tumors [2]. The 5-year relative survival rate of EC is 72.8%, and the prognosis varies greatly among different subtypes. In 1983, Bokhman proposed a dualistic model of EC; WHO's histological classification also divided EC into multiple subtypes such as endometrioid carcinoma, serous carcinoma, clear cell carcinoma, and mixed cell carcinoma. However, in clinical use, these two typing methods have their own limitations. Studies have also confirmed that there are differences between the prognosis of traditional clinicopathological risk groups and molecular classification, and some patients treated according to traditional methods are over-treated or under-treated[3].
Since the TCGA study in 2013, more and more evidence has shown that molecular typing has the value of prognostic prediction and individualized treatment of EC, and molecular typing has been included in the fifth edition of WHO classification of tumors of the female reproductive tract, NCCN guidelines for uterine tumors, ESGO /ESTRO/ESP and SGO and other authoritative guidelines for women's tumors in Europe and the United States. The domestic guidelines for the diagnosis and treatment of endometrial cancer (2021 edition) and the expert consensus on molecular detection of endometrial cancer (2021 edition) also recommend molecular typing for patients with EC [4-5]. NGS technology is a promising approach to enable large-scale genome sequencing, which may have advantages in terms of accuracy, time, and cost efficiency for molecular typing of EC.
Research methods
The retrospective cohort of this study consisted of 70 patients with grade 3 endometrioid carcinoma (EEC) treated in Fujian Cancer Hospital from June 2018 to May 2021, and most (85.7%) patients were < 60 years old. G3 EEC was diagnosed based on morphological features, and all HE sections were independently evaluated by two pathologists. Clinical and pathological data of the patients were collected, including age, tumor size, FIGO stage, lymph node status, and LVSI. The clinicopathological features and morphological features of each molecular subtype are shown in the original text, and all clinicopathological parameters were not significantly correlated with molecular subtypes (P >0.05).
NGS detection uses FFPE samples, and the 11-gene panel designed by XIAMEN SPACEGEN CO.,LTD., based on RingCap® amplicon library construction technology , the panel is designed for the POLE exonuclease domain, the entire coding region of TP53, MMR genes and the hotspot regions of some auxiliary typing genes, and includes MSI status detection. Sequencing was performed on the MiseqDx platform. The study also carried out IHC and MLH1 promoter methylation detection.
Research results
NGS analysis of 11 genes identified four molecular subtypes: POLE hypermutation (n = 20, 28.6%), MSI-H (n = 27, 38.6%), NSMP (n = 13, 18.6%), and TP53mut (n = 10, 14.3%), indicating a high degree of heterogeneity in the molecular subtypes of G3 EEC. The higher proportion of POLE hypermutated cases and lower proportion of p53abn cases in this study may be due to the younger age of patients at diagnosis, as seen in 257 young (<50 years old) female ECs from the ProMisE cohort.
Molecular typing based on POLE sequencing, MMR, and p53 IHC also identified four subtypes: POLE hypermutation (n = 20, 28.6%), MMRd (n = 26, 37.1%), NSMP (n = 14, 20% ) and p53mut (n = 10, 14.3%). The results of molecular typing of 70 G3 EECs using NGS panel and IHC are shown in the table below, and the consistency between NGS and IHC reached 98.6% (69/70). This is close to the previously reported 98.1% concordance between F1CDx and IHC.
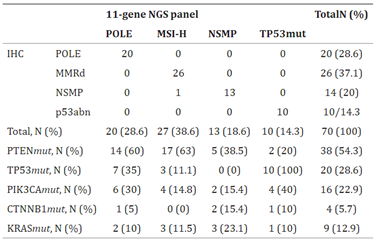
Molecular typing of 70 cases for G3 EEC
In addition to the typing markers, the pathogenic mutations of PTEN, TP53, PIK3CA, CTNNB1 and KRAS detected by NGS panel accounted for 54.3%, 28.6%, 22.9%, 5.7% and 12.9% of the total cases.
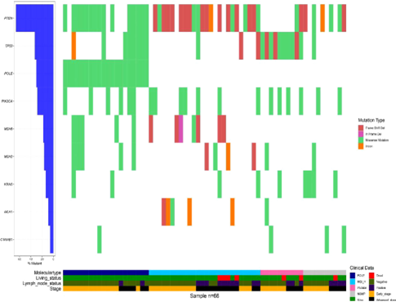
The mutation map of 70 cases for G3 EEC
POLE sequencing
Among the 20 cases of POLE hypermutation, the most common hotspot mutations (P286R and V411L) were found in 10 (50%) and 7 (35%) tumor samples, respectively. In addition, there were 1 case each for A456P, P436R, and Y473C. Similar to previous reports, the most common hotspot mutations (P286R and V411L) covered 85% of POLE hypermutation cases. Furthermore, high mutational burden and polymolecular features were observed in POLE hypermutation in 2 MMRd/MSH-H cases and 7 TP53mut/p53abn cases.
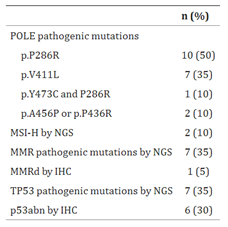
Molecular characterization of POLE hypermutants in G3 EEC
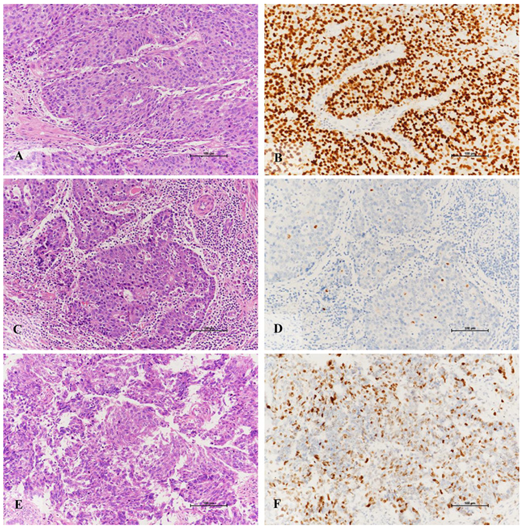
MSI/MM Detection
28 MSI-H (40%), 4 MSI-L (5.7%) and 38 MSS (54.3%) EECs were identified by NGS method.27 of 28 MSI-H tumors were classified as MSI-H, and only one tumor was classified as POLE hypermutated. Among these MSI-H tumors, 2 cases showed normal MMR staining by IHC and were classified as NSMP group. Further MLH1 methylation testing revealed that one of the two suspect cases was hypermethylated.
IHC characterization of MLH1 methylated EEC
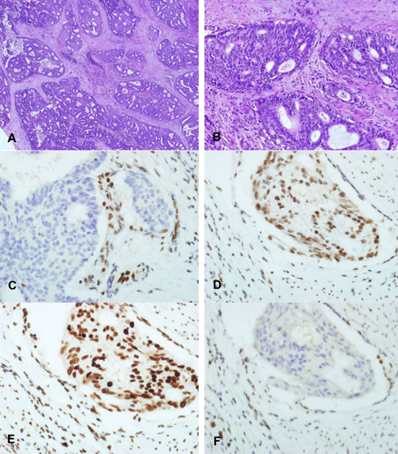
TP53/p53 Detection
20 cases (28.6%) of TP53 somatic pathogenic mutations were identified by NGS, including 10 cases of TP53mut type, 8 cases of POLE hypermutation type, and 2 cases of MSI-H type. Of these cases, 5 tumors showed normal p53 staining by IHC (3 cases with POLE hypermutation and 2 cases with MSI-H type). In addition, one POLE hypermutant sample was identified as TP53wt by NGS, but stained abnormally for p53 by IHC. Abnormal expression of p53 protein was observed by IHC in all cases in TP53mut type.
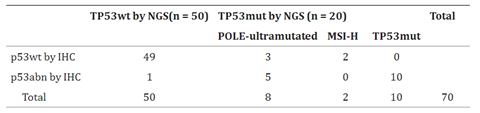
Comparison of TP53 (p53) status by NGS and IHC analysis
The 6 cases with TP53 mutation or discordant p53 staining were all multimolecular EC, which may be because more TP53 mutations could be identified by NGS compared with p53 IHC. TP53 mutation or abnormal expression in polymolecular type cases may be POLE mutation or secondary mutation of MMRd during tumor progression, which has been confirmed in previous findings. And TP53 mutation may not affect the expression of p53 protein. It was reported that the concordance between p53 IHC and TP53 mutations was 95.1% after excluding POLE hypermutated and MMRd types.
HC Characterization of TP53 Mutant EEC
Conclusion
In this study, the researchers performed NGS molecular typing on 70 cases of G3 EEC using the 11-gene panel of XIAMEN SPACEGEN CO.,LTD., and the consistency rate with the results assessed by IHC reached 98.6%. Among the 7 deaths, 4 were MSI-H tumors, 2 were TP53mut/p53abn tumors, and 1 was NSMP tumor. The average OS was 14.7 months. The TP53mut subgroup showed poorer OS, and the POLE hypermutated type had a better prognosis.
This study shows that XIAMEN SPACEGEN CO.,LTD .’s endometrial cancer molecular typing is suitable for EC molecular typing including G3 EEC, and can be used to guide prognosis and treatment decisions. Compared with IHC methods, NGS panel combined mutational and MSI analysis provided an efficient and accurate molecular classifier for EC.
Reference
[1] Front Oncol. 2022 Aug 8;12:935694.
[2] IARC's latest global cancer burden data for 2020
[3] Br J Cancer. 2015 Jul 14;113(2):299-310.
[4] Guidelines for the diagnosis and treatment of endometrial cancer (2021 edition)
[5] Expert consensus on molecular detection of endometrial cancer (2021 edition)