Current location: Home > NEWS > Industry news
NEWS
PRODUCTS
Cervical cancer "early warning assistant" - gene methylation
News source: Release time:[2022-12-05]
Cervical cancer is one of the common malignant tumors among women in China, with the second highest incidence rate among gynecologic malignancies, after breast cancer. 110,000 new cases of cervical cancer and 59,000 deaths occurred in China in 2020, with a slightly higher incidence rate in rural areas than in urban areas, and a higher incidence rate in central and western regions than in eastern regions [1]. The median age of onset of cervical cancer patients in China is mostly 40-50 years old. However, in recent years, the average age of cervical cancer incidence is gradually decreasing and there is a trend towards younger age [2].
Cervical cancer and human papillomavirus (HPV) has a close relationship between the two. Studies have shown that persistent infection with high-risk HPV (HR-HPV) is necessary to cause cervical cancer. Despite this, it is not the case that infection with HR-HPV leads to the development of cervical cancer (the majority of women can rest assured, see below for more details).The main reason is that less than 10% of women develop cervical cancer or cervical intraepithelial neoplasia (CIN) despite a lifetime probability of more than 70% of HR-HPV infection, mainly because 80% of women have a transient HPV infection [2] (i.e., autoimmunity clears HPV and does not allow HPV to grow in the body so that it does not lead to cervical cancer)
HPV DNA + liquid-based thin-layer cytology (TCT) testing is currently the main tool for cervical cancer screening, but both testing techniques have certain shortcomings [3]. HPV DNA testing has low specificity in identifying precancerous lesions (due to the apparent transient nature of HPV infection in most women) and tends to cause excessive colposcopy referrals, resulting in psychological fear among women. TCT testing, on the other hand, relies on the quality of the film and the physician's experience in reading it, which can easily lead to improper risk stratification for precancerous lesions or missed diagnosis of cervical cancer (especially cervical adenocarcinoma, which is mostly asymptomatic, multifocal, and not easily diagnosed). From this perspective, it would be a real boon for the early detection of cervical cancer by our fellow women if there is a technology that can both identify cervical precancerous lesions more accurately and avoid overdiagnosis and underdiagnosis. At the right time, genetic methylation testing technology was born.
Gene methylation is a chemical modification process in which S-adenosylmethionine (SAM) is transferred as a methyl donor to the C5 position of cytosine to form 5-methylcytosine in the presence of DNA methyltransferase (DNMT) (Figure 2). Numerous studies have shown that this modification pathway is closely related to the regulation of gene expression. dna methylation turns off the activity of certain genes and demethylation induces reactivation and expression of genes. dna methylation can cause changes in chromatin structure, dna conformation, dna stability and the way dna interacts with proteins, thus controlling gene expression.
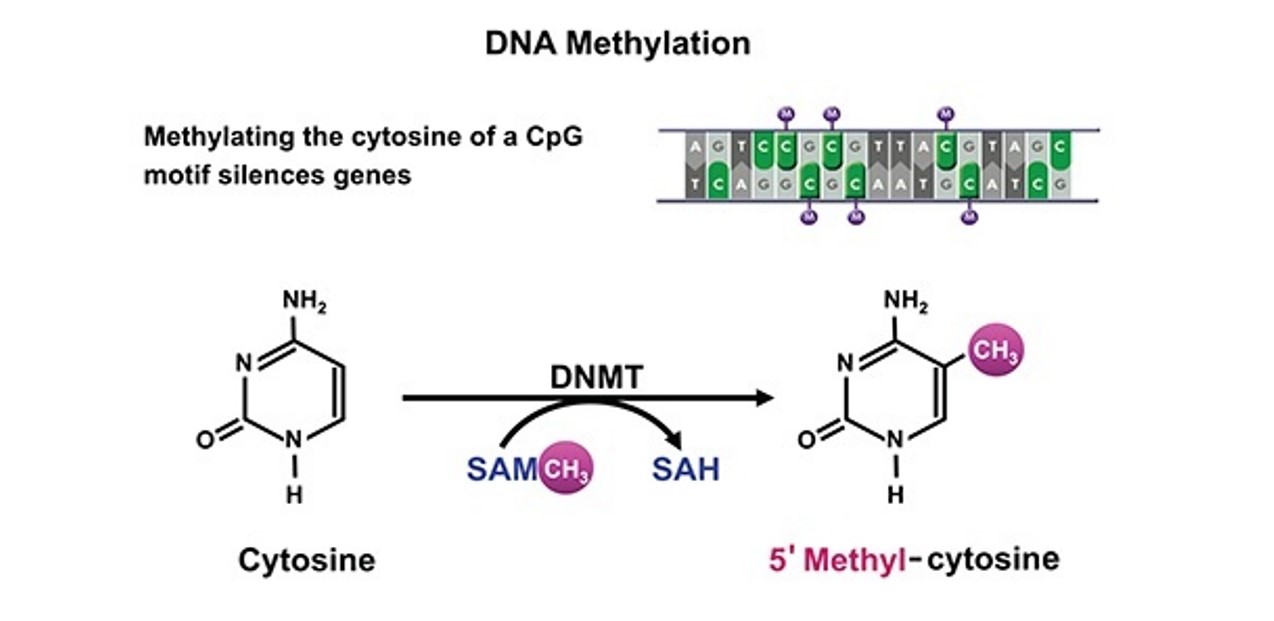
▲Figure 2 Gene methylation
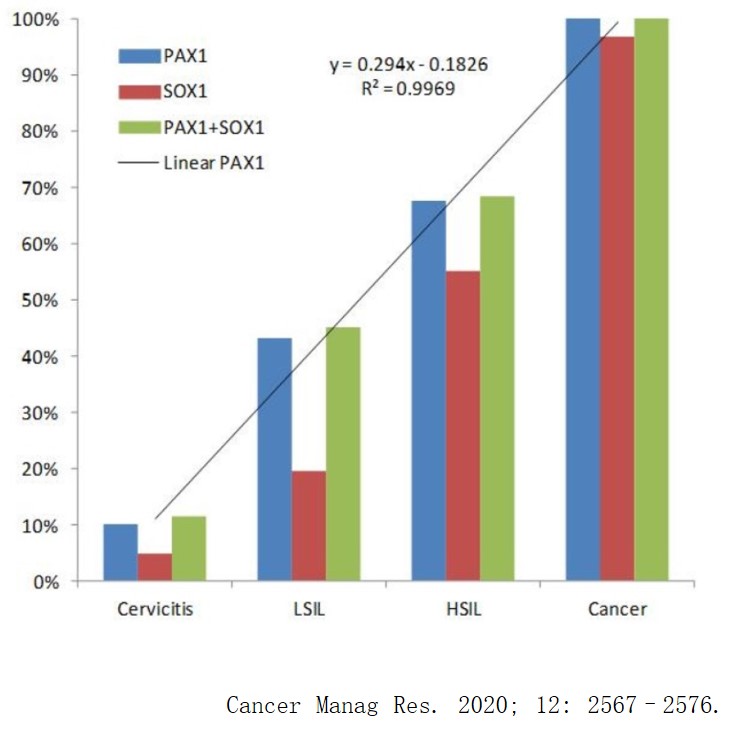
The degree of PAX1 gene methylation is closely associated with the progression of cervical cancer [4] (Figure 3). As early as 2008, Lai et al. found abnormal methylation of PAX1 gene in cervical cancer [5]; in 2010, Lim et al. showed that the methylation level of PAX1 gene gradually increased with the degree of cervical lesions [6]; in 2015, Nikolaidis et al. used PAX1 gene methylation for the assessment of CIN II and CIN III, and the results showed that PAX1 gene methylation better improves the sensitivity and specificity of cervical cancer screening [7]. Numerous studies have shown that PAX1 gene methylation is a veritable "early warning aid" for cervical cancer, as it can detect early pre-cancerous high-grade and above lesions (HSIL+) and also shows significant value in the triage of ASC-US patients.
01
More accurate detection of precancerous cervical lesions
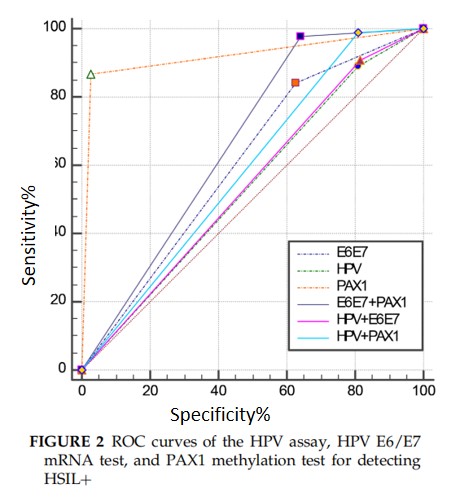
A retrospective study of 337 patients with cervical lesions showed [8] that the PAX1 gene methylation test had the largest AUC for the diagnosis of HSIL+ (0.919), significantly higher than the HPV E6/E7 mRNA test (AUC=0.607) and HR-HPV test (AUC=0. 541).PAX1 gene methylation has a high specificity and can be an important future screening tool, but also as a combined screening tool for earlier and more accurate detection of cancer.
02
ASC-US diversion
A study of 463 TCT cases with ASC-US results showed [9] that the specificity and sensitivity of PAX1 methylation were 95.6% and 82.4%, respectively, while the specificity and sensitivity of HPV DNA testing were 59.7% and 64.7%, respectively .PAX1 methylation testing can be applied to ASC-US triage, screen out high-risk groups (CIN2+), avoid missed or overdiagnosed cases, and reduce colposcopy referral rates and patient psychological anxiety and burden (Figure 5).
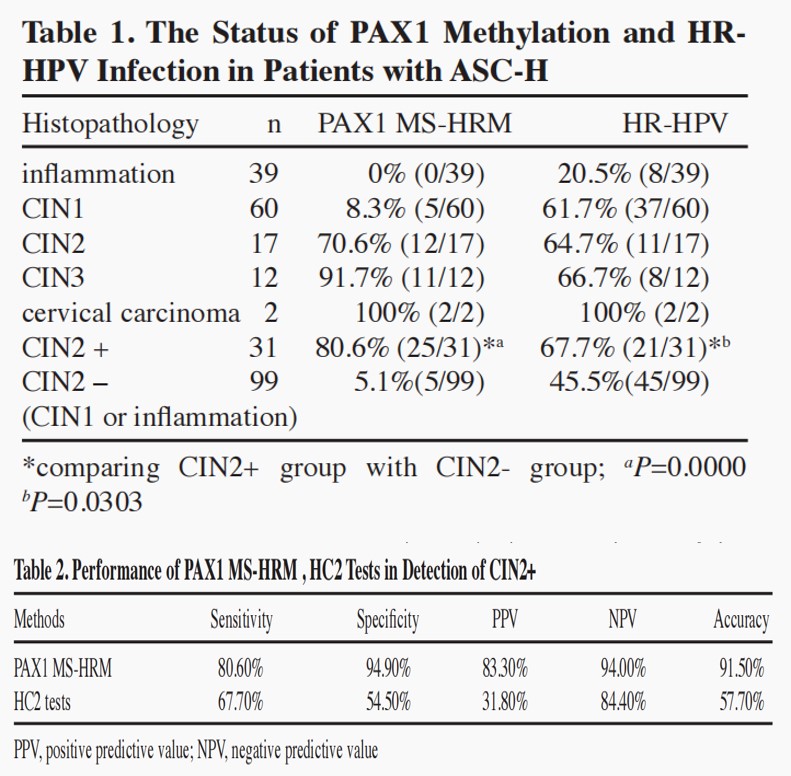
▲Figure 5 Study of 463 TCT cases with ASC-US test results
In addition, PAX1 gene methylation has the potential to become an "all-rounder" in terms of avoiding missed diagnosis and monitoring the efficacy of cervical cancer.
03
Avoiding missed diagnosis of adenocarcinoma
It was shown [10] that the level of PAX1 gene methylation in adenocarcinoma was much higher than in normal controls. The results of tissue samples showed that PAX1 hypermethylation developed into adenocarcinoma OR=15.7 (7.0-40.6, P<0.001), and the results of cervical exfoliated cell samples showed that PAX1 hypermethylation developed into adenocarcinoma OR=6.2 (2.6-15.4, P<0.001) (Figure 6).
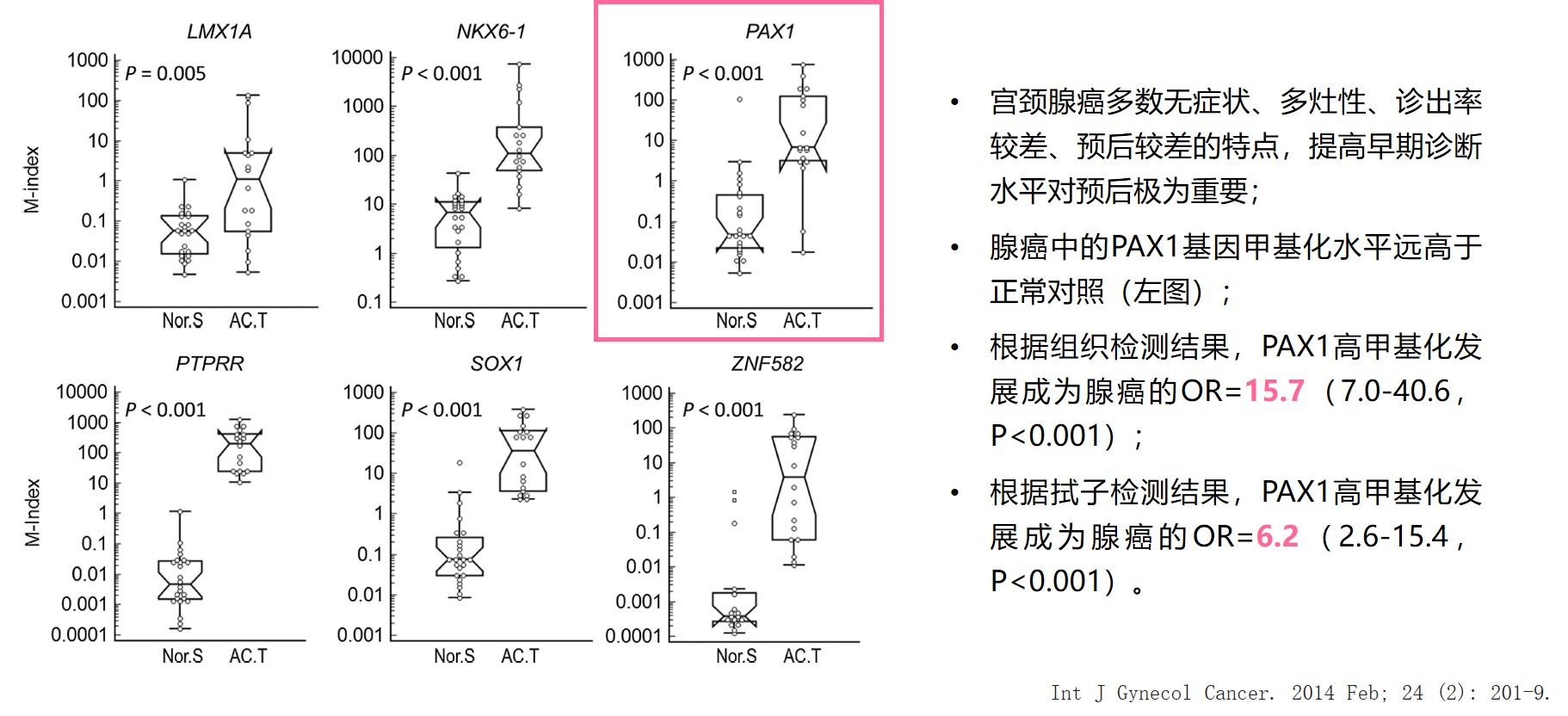
▲Figure 6 Cervical adenocarcinoma study
04
Monitoring
A study of 82 hypermethylated cervical cancer patients monitored for the effects of synchronous radiotherapy [11] showed that PAX1 gene methylation levels predicted the sensitivity and efficacy of synchronous radiotherapy in cervical cancer and that PAX1 gene methylation levels better reflected early molecular changes in the tumor during treatment than MRI parameters (Figure 7).
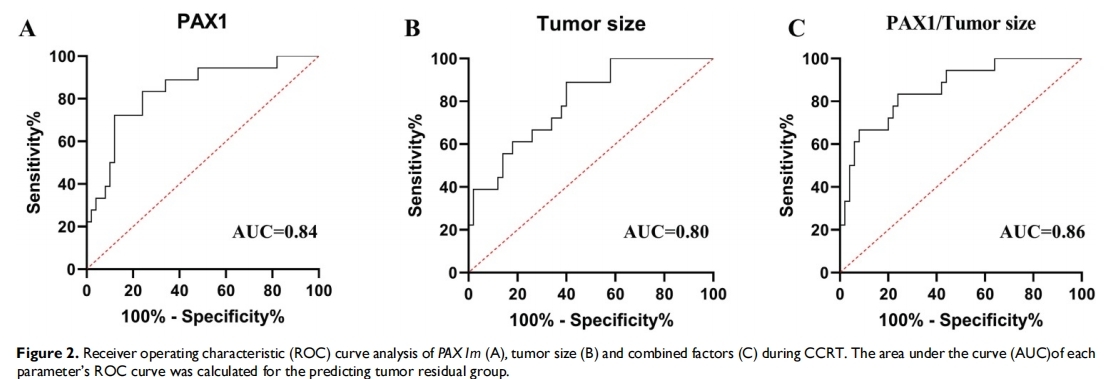
Figure 7 Study of the effect of monitoring simultaneous radiotherapy in 82 patients with hypermethylated cervical cancer
Cervical cancer is currently the only cancer with a clear cause that can be eradicated through early prevention, screening, and treatment.WHO proposed the Global Strategy for Accelerated Elimination of Cervical Cancer in 2020, aiming to achieve the 90-70-90 target by 2030 [12], which is.
1. 90% of girls complete HPV vaccination by age 15 years;
2. 70% of women are screened by highly effective testing methods by age 35 and again at age 45;
3. 90% of women with cervical disease are treated.
Also, WHO has proposed a three-tier strategy for global prevention and control of cervical cancer [12] (Figure 8) to guide the accelerated eradication of cervical cancer. Among the prevention and control strategies, high-quality cervical cancer screening modalities have shown some importance as secondary prevention strategies. The current HPV DNA+TCT cervical cancer screening modality suffers from lack of precision, excessive colposcopic referral and biopsy, and waste of medical resources, and is in urgent need of new technologies to complement it. Gene methylation testing technology has shown excellent clinical value, and we expect the new technology to help the prevention and treatment of cervical cancer in China and the world.
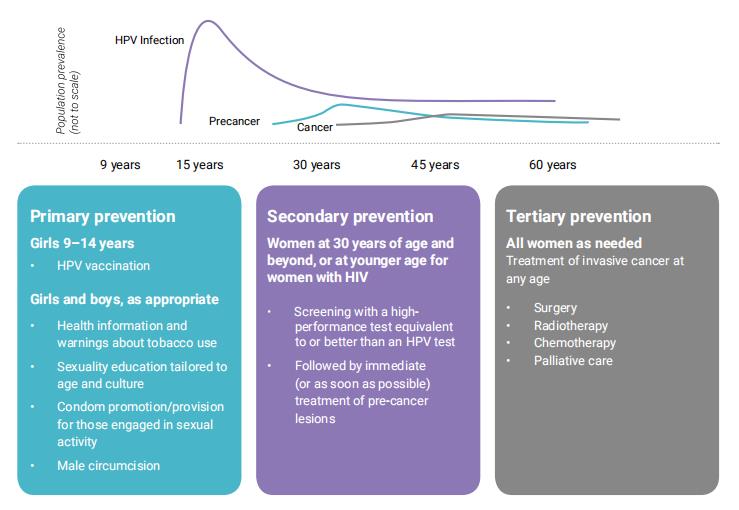
▲Figure 8 Global three-tier strategy for prevention and control of cervical cancer