Current location: Home > NEWS > Industry news
NEWS
PRODUCTS
CAR-T cells: Alter Patients' Immune Cells to Treat Cancer
News source: Release time:[2022-04-21]
For decades, cancer treatment has been dominated by surgery, chemotherapy and radiation therapy. These remain key treatments, but recently new treatments have helped transform how cancer patients are treated.
1.CAR-T cell therapy is widely used
In the early 21st century, targeted therapies such as imatinib (Gleevec) and trastuzumab (Herceptin) appeared one after another. The two drugs find and kill cancer cells by tracking specific molecular changes found primarily in cancer cells, and dozens of targeted therapies are now standard treatments for many cancers.
Over the past decade, immunotherapy, which boosts a patient's immune system's ability to attack tumors, has quickly become what many call the "fifth pillar" of cancer treatment. That's because drugs that boost the immune system have shown the ability to shrink or even eradicate tumors in some advanced cancer patients. In a small percentage of patients, these treatment responses can last for years.
For example, drugs called immune checkpoint inhibitors are already widely used to treat a variety of cancers, including melanoma, lung, kidney, bladder and lymphoma.
But another form of immunotherapy, called CAR-T cell therapy, although CAR-T cell therapy is not as widely available as immune checkpoint inhibitors, they have shown the same ability to eradicate end-stage leukemia and lymphoma tumor and inhibit cancer recurrence for many years.
Since 2017, the U.S. Food and Drug Administration (FDA) has approved six CAR-T cell therapies. All are approved to treat blood cancers, including lymphoma, some forms of leukemia, and multiple myeloma. Despite the encouraging efficacy of these drug treatments, less than half of the patients treated survive long-term.
Dr. Rosenberg said: "(CAR-T cells) are now widely available in the United States and other countries and have become a standard of care for patients with aggressive lymphomas. They have become part of modern medicine."
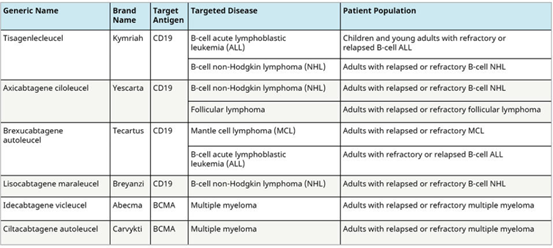
▲FDA-approved CAR-T studies
2.AR-T cell therapy: a "living drug"
As the name suggests, T cells that help coordinate immune responses and directly kill pathogen-infected cells are the backbone of CAR-T cell therapy.
Currently available CAR-T cell therapy is tailored to each patient. They are made by harvesting T cells from patients and reconstituting them in the laboratory to produce proteins on their surface called chimeric antigen receptors (CARs), which recognize and bind to specific cells on the surface of cancer cells protein or antigen.
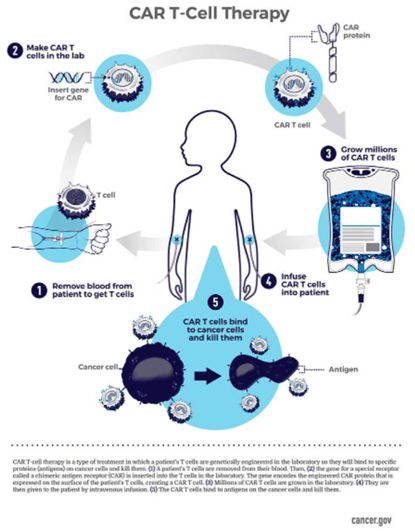
▲CAR recognizes and binds to specific proteins or antigens on the surface of cancer cells
3. More than just CAR-T cells: TILs and TCRs
In cell therapy, CAR-T cells have gained the most attention. But other types of cell therapy have also shown promise in small clinical trials, including in patients with solid tumors.
One of these, called tumor-infiltrating lymphocytes (TILs), uses immune cells that have infiltrated the tumor's interior and surrounding environment. NCI researchers have pioneered the use of TILs to successfully treat patients with advanced cancer, initially with melanoma and later with several other cancers, including cervical cancer. Recently, NCI researchers developed a technology to identify TILs that can identify cancer cells with mutations specific to that cancer exit disclaimer and identify people whose cancers are more likely to respond to TIL therapy.
Another type of cell therapy involves engineering a patient's T cells to express specific T cell receptors (TCRs). Unlike CARs, the partially synthetic antibodies used by TCRs can only recognize specific antigens on the cell surface, while the natural receptors used by TCRs can also recognize antigens inside tumor cells.
So far, TCR-T cells have been tested in patients with a variety of solid tumors, showing promising results in melanoma and sarcoma.
▲Natural receptors used by TCRs recognize antigens in tumor cells
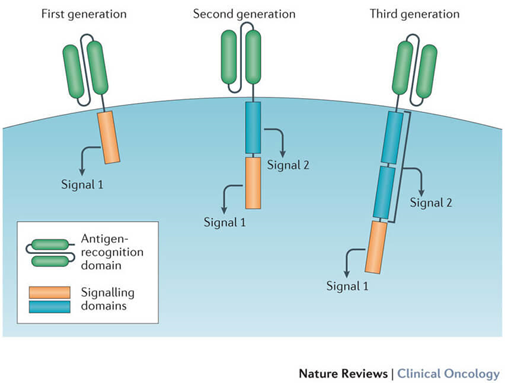
A costimulatory signaling domain has been added to the new generation of CAR-T cells to improve their ability to generate more T cells after infusion and survive longer in the circulation.
Reference:https://www.cancer.gov/about-cancer/treatment/research/car-t-cells